HOW TO BOOST YOUR IMMUNE SYSTEM AND MODULATE THE CYTOKINE STORM IN VIRAL INFECTIONS
Coronavirus disease (COVID-19) is an infectious disease caused by a new coronavirus SARS-CoV-2.
Most people infected with the COVID-19 virus will experience mild to moderate respiratory illness.
Older people, and those with underlying medical problems like cardiovascular disease, diabetes, chronic respiratory disease, and cancer are more likely to develop serious illness.
Factors that make us more likely to contract COVID-19:
- Cardiovascular disease
- Diabetes
- Age
- Hypertension
- Obesity
- Chronic pulmonary disease
- Chronic liver or kidney disease
- Autoimmune conditions
- Chronic neurological diseases
Statistics about comorbidities:
71% of those hospitalized with COVID-19 in the United States and 78% of those in intensive care have underlying health conditions like diabetes, heart disease, and chronic lung disease.
Source:
CDC.gov, March 28, 2020
COVID-19 and Heart Health:
COVID-19 is associated with high inflammatory burden that can induce vascular inflammation, myocarditis, and cardiac arrhythmia.
Source:
Tao G, Yong Zhen F, Ming C, et al. JAMA Cardiol, Mar 27, 2020 (Online)
Early Signs of Infection:
Loss of smell or taste might be an early sign of infection with coronavirus SARS-CoV-2.
Incubation Period:
New study on COVID-19 estimates 5.1 days for the incubation period.
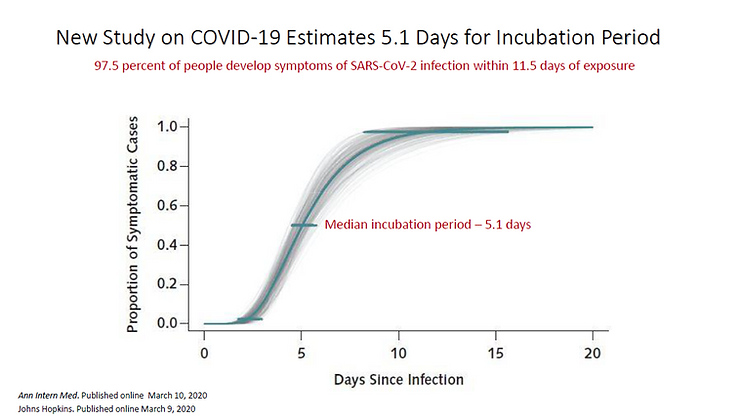
Source: Ann Intern Med. Published online March 10, 2020, Johns Hopkins. Published online March 9, 2020
Ibuprofen and COVID-19:
Ibuprofen is not recommended for use in COVID-19 because it damages the gut lining and the tight junctions of the blood-brain barrier. Ibuprofen also increases Angiotensin-converting enzyme 2 (ACE2).
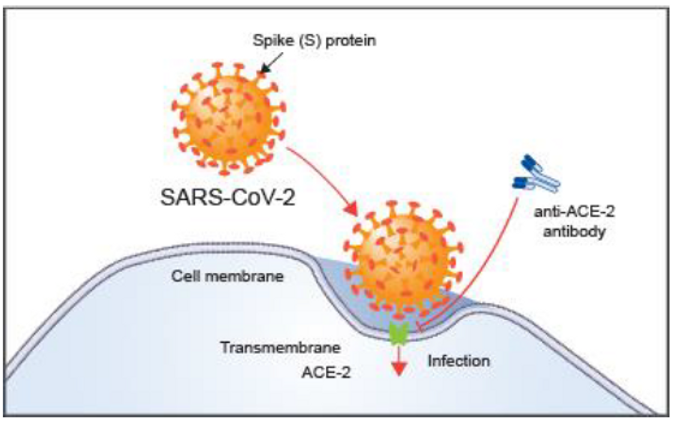
What is ACE2?
Angiotensin-converting enzyme 2 (ACE2) is an enzyme attached to the outer surface of cells in the lungs, heart, arteries, kidneys, and intestines. ACE2 lowers blood pressure and also serves as the entry point into cells for some coronaviruses.
Source:
“Gene: ACE2, angiotensin I converting enzyme 2”. National Center for Biotechnology Information (NCBI), U.S. National Library of Medicine. 2020-02-28.
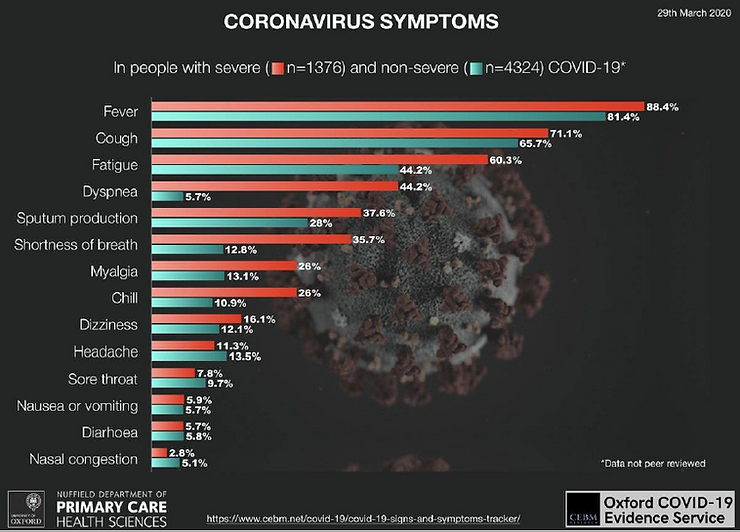
Coronavirus Symptoms:
- Fever
- Cough
- Fatigue
- Dyspnea
- Sputum production
- Shortness of breath
- Myalgia
- Chills
- Dizziness
- Headache
- Sore throat
- Nausea or vomiting
- Diarrhea
- Nasal congestion
Ocular abnormalities can also appear in COVID-19 patients, involving:
- Eye conjunctivitis
- Conjunctival hyperemia
- Epiphora
- Chemosis
- Increased secretions
These ocular abnormalities repeatedly occurred in patients with more severe COVID-19.
Source:
Wu P, Duan F, Luo C, et al. Characteristics of Ocular Findings of Patients With Coronavirus Disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. Published online March 31, 2020
Why Does SARS-CoV-2 Spread So Easily?
Coronavirus can make 10,000 copies of itself in just a few hours. Within a few days, an infected patient can have hundreds of millions of viral particles in every teaspoon of blood.
Source: Medical News Today
ACE-2 and SARS-CoV-2
- ACE-2 is the host cell receptor responsible for mediating infection by SARS-CoV-2, the coronavirus responsible for COVID-19.
- SARS-CoV-2 has a specific structure that allows it to bind at least 10 times more tightly than the corresponding spike protein of SARS-CoV to their common host cell receptor.
- SARS-CoV-2 binds to ACE2 with higher affinity than other coronaviruses, making it 10 times more effective at binding to host cells than SARS-CoV.
- Treatment with anti-ACE-2 antibodies disrupts the interaction between the virus and receptor.
Source: R&D Systems
Fecal and oral transmission may be part of the COVID-19 clinical picture.
10% of coronavirus patients experience GI symptoms such as:
- Diarrhea
- Nausea
- Vomiting
- Abdominal discomfort
These symptoms often appear before the onset of respiratory symptoms.
Researchers have found that RNA and proteins from SARS-CoV-2 (the viral cause of COVID-19) are shed in feces early in infection and persist even after respiratory symptoms subside.
GI manifestations are consistent with the distribution of ACE2 receptors, which serve as entry points for SARS-CoV-2.
These receptors are most abundant in the cell membranes of lung AT2 cells and in enterocytes in the ileum and colon.
GI Tract as a Possible Route of Viral Transmission:
- 53.4% of patients had SARS-CoV-2 RNA detected in stool samples.
- 23% of patients tested positive in stool despite testing negative for the virus in respiratory samples.
- Clinical evidence suggests the digestive system may serve as an alternative route for SARS-CoV-2 infection.
- In addition to the respiratory tract, clinicians should be vigilant in identifying patients with initial GI symptoms.
Source: Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for gastrointestinal infection of SARS-CoV-2, Gastroenterology, Feb. 27, 2020 online.
GUT-LUNG CONNECTION
Dr. Rob’s GUT MATRIX
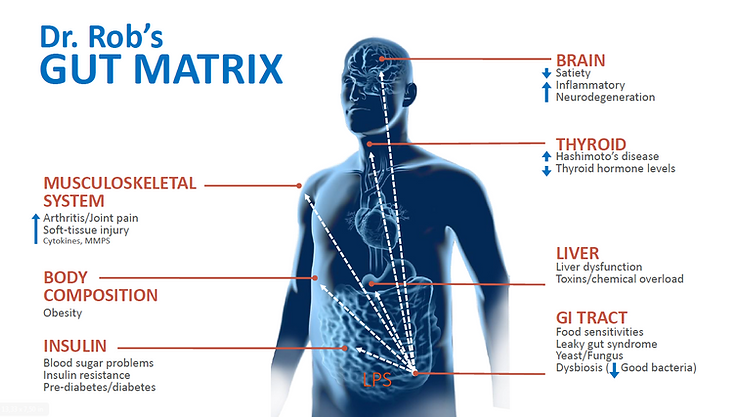
“Your gut is not Las Vegas. What happens in the gut does not stay in the gut.” – Dr. Alessio Fasano (Italian medical doctor, pediatric gastroenterologist, and researcher).
What happens in the gut doesn’t stay in the gut.
The gut affects your:
- Brain
- Thyroid
- Lungs
- Liver
- Digestion
- Immunity
- Weight
- Skin
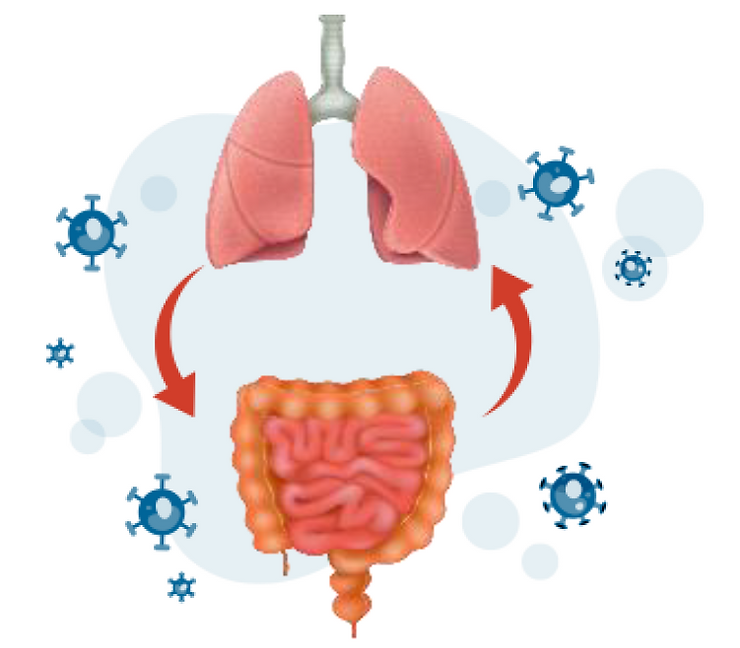
GUT-LUNG CONNECTION
Lungs should be considered an ecosystem with their own microbiota.
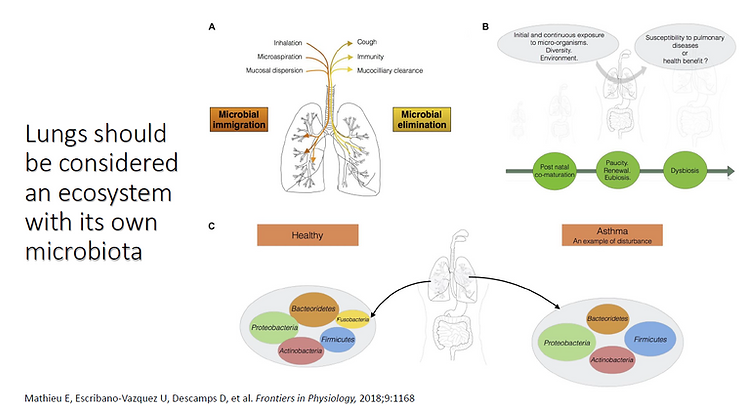
References:
- Mathieu E, Escribano-Vazquez U, Descamps D, et al. Frontiers in Physiology, 2018;9:1168
- Negi S, Pahari S, Bashir H, Agrewala JN. Frontiers in Immunology, 2019;10:1142
- Zhu X, Han Y, Du J, et al. OncoTarget. 2017 May 10;8(32):53829-53838
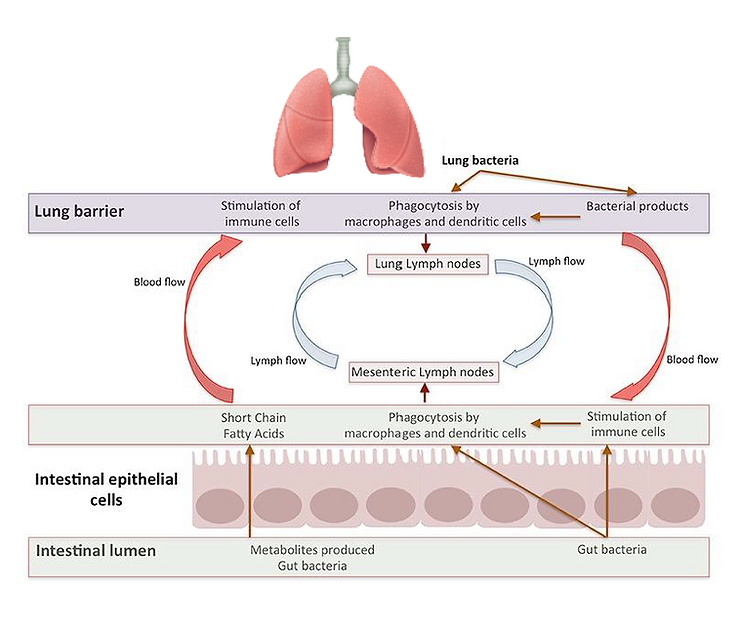
Gut-Lung Communication
The gut microbiota feeds and matures the intestinal epithelium and is involved in immunity, while the principal role of the lung microbiota seems to be the orientation and balance of aspects of immune and epithelial responsiveness. This implies that the local and remote effects of bacterial communities are likely to be determinants in many respiratory diseases caused by viruses, allergens, or genetic deficiency.
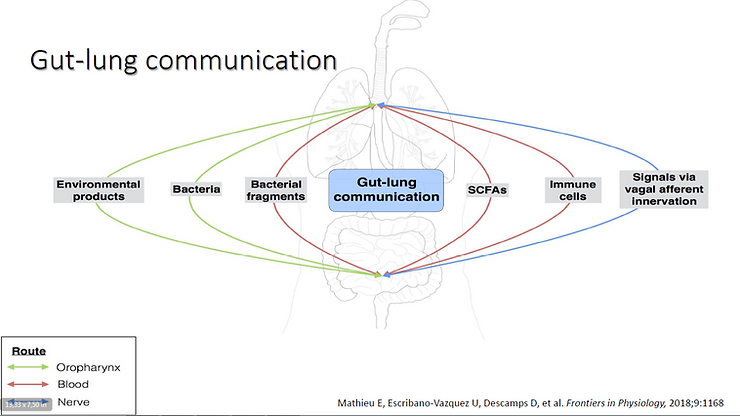
The gut–lung axis (GLA) has emerged as a specific axis with intensive dialogues between the gut and lungs. It comprises the anatomical, systemic, and nervous system connections mediating reciprocal exchanges of microbial signals between the lungs and the gut.
One of the connections between the gut and the lung involves the translocation of bacteria via oropharynx reflux. The human body experiences multiple reflux events (especially in pathological conditions) that can transport different bacterial communities from the digestive tract to the upper respiratory tract. The bacteria can then be translocated to the lungs by micro-aspiration. Bacteria and bacterial fragments may also be translocated in the lymph and blood, as both play a significant role in the migration of immune cells to distal sites.
Reference:
- Mathieu E, Escribano-Vazquez U, Descamps D, et al. Frontiers in Physiology, 2018;9:1168
Bidirectional Gut-Lung Axis
Soap breaks up the membrane of the virus and deactivates it. Wash your hands often for 20 seconds or more.
To Protect Yourself from COVID-19, You Need to Support Your Immune System.
To Boost Your Immune System, Avoid Certain Foods:
- Gluten – Damages your gut. Dr. Silverman says, “Never been a better time to start being gluten-free.” Many research studies have linked gluten to intestinal permeability. Gluten directly impacts the intestinal lining through zonulin production, causing leaky gut, which contributes to autoimmune disease.
- Processed food
- Sugar
- Artificial sweeteners – May change gut bacteria balance and cause leaky gut.
- Dairy – A highly allergenic food that damages the gut and increases mucus production.
- Detect and avoid food sensitivities.
Proper Diet Leads to Enhanced Immunity. Poor Diet Causes Impaired Immunity.
Healthy Diet to Boost Your Immune System:
- Plant-based diet: Vegetables and fruits – rich in antioxidants, vitamins, and minerals.
- Wild fish: Salmon, mackerel, anchovy, sardines, herring.
- Grass-fed meats.
- Chicken soup and bone broth.
- High fiber – fiber is a prebiotic that feeds good bacteria for gut health.
- Snack – organic dark chocolate.
- Herbals – ginger, turmeric.
- Oils – olive oil, avocado, macadamia nut oil.
- Mushrooms – shiitake, reishi, turkey tail, maitake, oyster, lion’s mane.
- Nuts, avocado, olive oil – Oleic acid (omega-9 fatty acid) from these foods stimulates SIRT1, a defense enzyme.
- Appropriate fluid intake – hydration is essential for health.
Lifestyle Changes to Boost Your Immune System:
- Time-restrictive eating or intermittent fasting – fast for 12-16 hours.
- Get sufficient sleep – 7-8 hours of good quality sleep to improve the immune system.
- Humidity – maintain home humidity for airway health and mucus.
- Exercise – improves sleep quality and duration.
Immune Support Supplements:
- Vitamin C – Liposomal vitamin C is the best form.
- Vitamin D3 with K2 – 5000-10,000 IU D3.
- Zinc – 20 mg/day helps the immune system fight viral infections by inhibiting viral replication.
- Mixed mushroom complex – supports immune function.
- Probiotics.
- Liposomal glutathione – the master antioxidant.
- Beta-glucans.
- Omega-3 fatty acids.
- Elderberry.
Role of Vitamin C in the Body
Vitamin C is the main systemic extracellular antioxidant. High doses (3-10 g/day orally or 10-50 g/day IV) function as antioxidants to prevent toxicity from reactive oxygen species (ROS) and viruses. It supports intracellular antioxidants like glutathione (GSH) and catalase.
Vitamin C empowers the immune system, promoting chemotaxis, growth, and activity of immune cells (macrophages, lymphocytes, natural killer cells), aiding the body in fighting infections.
Prevention of Viral Infections:- Most individuals tolerate 1000-3000 mg/day in divided oral doses to maintain stable levels in the bloodstream.
- High levels of vitamin C lower the risk of viral infections by assisting immune function.
- Oral doses of vitamin C can directly denature viruses.
Liposomal Vitamin C
Liposomal vitamin C is absorbed differently in the gut, binding directly to gut cells and bypassing active transport. It allows for a higher level of absorption than regular vitamin C. Taking both forms together increases bloodstream levels.
Vitamin D
Vitamin D deficiency is associated with an increased risk of viral acute respiratory infections (ARI). Studies suggest that 2000-5000 IU/day of vitamin D helps prevent viral infections. Levels are lowest in winter and early spring – peak flu season.
Hospitalized pneumonia patients often have severe vitamin D deficiencies.
References:
- Gropper SS, Smith JL. (2013) Advanced Nutrition and Human Metabolism, 6th Ed. Wadsworth, Cengage Learning. ISBN-13: 9781133104056.
- Levy TE. (2011) Primal Panacea. Medfox Pub. ISBN-13: 978-0983772804.
- Orthomolecular Medicine News Service, Apr 3, 2020, “Rationale for Vitamin C Treatment of COVID-19 and Other Viruses”.
- Orthomolecular.org
- Orthomolecular Medicine Resources