Dr. Emeran Mayer on the Gut-Brain Connection
Dr. Emeran Mayer, executive director of the UCLA Center for Neurobiology of Stress, states that there is a connection between the gut and mental health conditions such as depression.
Many neuroscientists now call the gut a “second brain”.
In his book, The Mind-Gut Connection, Dr. Mayer writes: “Your gut has capabilities that surpass all our other organs and even rival your brain. It has its own nervous system, known in scientific literature as the enteric nervous system (ENS), and is often referred to in the media as the ‘second brain.’”
The Gut and Neurotransmitters
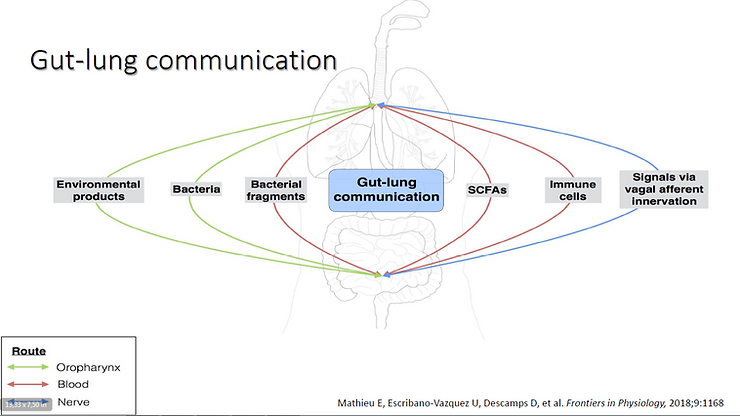
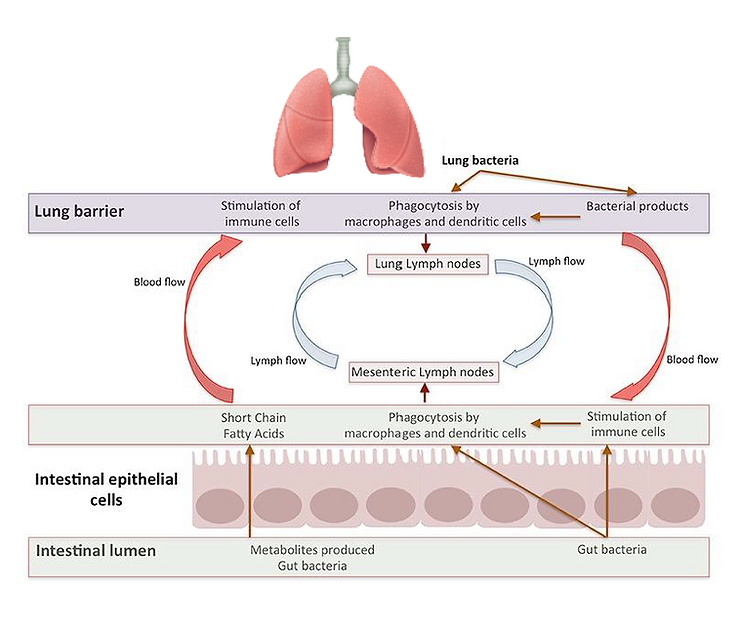
The gut consists of about 100 million nerve cells. This ‘second brain’ and our regular brain use the same neurotransmitters and are connected through neural, immune, and endocrine pathways. This creates an integrated intelligent system where information flows in both directions.
Scientists from the University of North Carolina have discovered that gut bacteria produce neurotransmitters like dopamine, serotonin, and GABA, which are all associated with mood regulation.
Another remarkable finding is that more than 95% of the body’s serotonin is produced and stored in the gut in specialized enterochromaffin cells.
Dr. Mayer states: “By far, the largest store of the molecule that plays such a big role in modulating our mood and our well-being—also appetite and pain sensitivity—is stored in the gut.”
The Microbiome and Mental Health
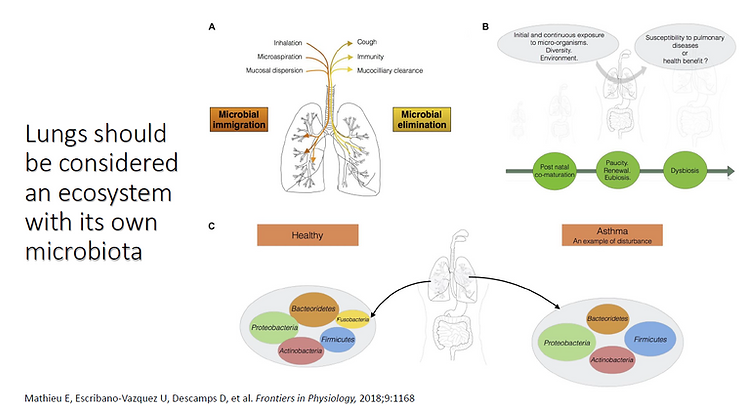
Studies suggest that our microbiome plays a crucial role in mental health and neurological conditions such as autism, epilepsy, and depression. Gut bacteria interact with the nervous system and release molecules that may even reach the brain.
Chronic stress and depression can reshape the gut bacteria’s composition by triggering stress hormones and inflammation. In turn, gut bacteria release toxins, metabolites, and neurohormones that can alter mood and eating behavior. Probiotic supplementation may help counteract these effects.
Factors Influencing Mood Disorders
Several factors contribute to mood disorders, including:
– Lack of sunlight
– Poor diet high in processed foods and sugar
– nnEMF (electromagnetic field) exposure
– Sedentary lifestyle
– Chronic stress and inflammation
– Chronic infections (e.g., Mycoplasma, Candida, parasites)
– Mitochondrial dysfunction
– Microbiome imbalance
– Exposure to chemicals and heavy metals
– Metabolic imbalances (hormones, micronutrients, dysglycemia)
– Epigenetic factors (e.g., MTHFR, MAO, COMT SNPs)
– Sleep disruption
– Overstimulation from smartphones and social media
Heavy Metals and Mental Health
Scientific evidence links heavy metal exposure to mental health conditions. For example:
– Mercury: Found in dental amalgam fillings, linked to depression, anxiety, and chronic fatigue.
– Aluminum: Associated with neurological problems, thyroid dysfunction, and memory loss. Common sources include cooking pots, aluminum foil, canned drinks, and deodorants.
– Lead: Causes depression and migraines. Found in hair dyes, lipsticks, inks, pesticides, and industrial paints.
Essential minerals help detoxify heavy metals:
– Magnesium and silicon neutralize aluminum.
– Zinc and selenium neutralize mercury.
– Iodine removes excess fluoride and BPA.
– Zinc and vitamin C help lower copper levels, which are linked to anxiety.
Testing for Mineral and Heavy Metal Imbalance
A hair analysis test is a reliable way to detect nutrient minerals and toxic metals in the body. Unlike blood tests, which regulate mineral levels at the expense of tissue reserves, hair analysis provides a more accurate representation of long-term mineral storage.
Circadian Rhythm and Mental Health
Circadian disruption is associated with mental disorders like major depressive disorder and bipolar disorder. The biological clock, discovered by American chronobiologists Jeffrey C. Hall, Michael Rosbash, and Michael W. Young, regulates hormone secretion, sleep quality, metabolism, and blood pressure.
Long-term circadian disruption can shrink the brain, contribute to neurodegenerative changes, and compromise the integrity of the intestines and the blood-brain barrier.
Chronic Infections and Mental Health
Chronic infections, such as yeast and parasitic infections, have been linked to mental illness:
– Candida releases neurotoxic byproducts like acetaldehyde.
– Toxoplasma gondii has been suspected of altering human behavior and contributing to schizophrenia.
Neuro-parasitology is an emerging science that explores how parasites manipulate the nervous system and influence host behavior.
Diet and Mental Health
Diet has a profound impact on mental well-being. Dr. Perlmutter explains:
“Food is far more important than just fuel. It is information. Food directly communicates with our bodies, our brains, and even our DNA. It determines whether we experience vibrant health or suffer from chronic disease. When it comes to cognitive health, the food we eat influences both the structure of our brains and how well they function.”
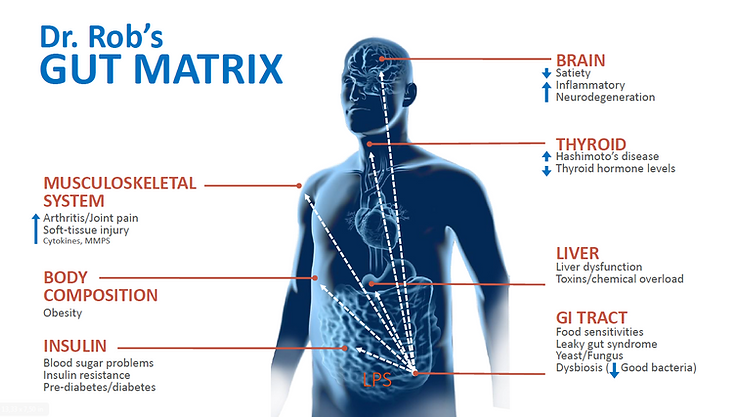
Poor diet, exposure to pesticides, antibiotics, and food additives disrupt the gut microbiome, leading to imbalances that can contribute to mental health disorders.
Gluten and Depression
Gluten elimination may be an effective treatment for mood disorders in individuals with gluten-related issues. Dr. Osborne explains:
“Many are unaware of the connection between gluten and depression. Gluten contributes to intestinal permeability (leaky gut), which allows harmful bacterial byproducts like LPS (lipopolysaccharide) to enter the bloodstream. This triggers inflammation, which alters brain function and can lead to depression.”
Gluten has also been linked to a disrupted blood-brain barrier (leaky brain), increasing susceptibility to neurological disorders.
Improving Mental Health Naturally
To enhance mental health and well-being, consider the following:
– Adopt a nutrient-dense diet
– Reduce inflammation
– Address chronic infections
– Restore gut health
– Balance hormones
– Detoxify the body
– Supplement with high-quality vitamins, minerals, and probiotics
– Practice stress management techniques
Get Personalized Support
If you are looking to improve your mood and overall well-being, I invite you to book a nutritional consultation, including a hair analysis test.
Certified Functional Medicine Practitioner
Katarzyna Blochowiak
www.diet-designer.com
Email: contact@diet-designer.com
Phone: 07707929982
Disclaimer of Medical Advice
All content provided is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a healthcare provider with any questions regarding your health.